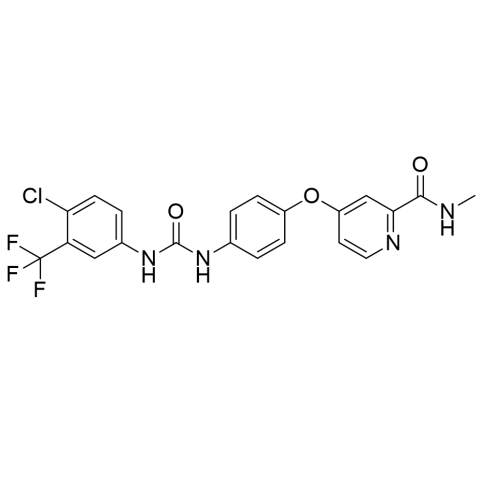
Sorafenib was developed by Bayer Pharmaceuticals over a period of 11 years, from initial screening to its FDA approval in December 2005 for advanced renal cell carcinoma. Originally known as BAY 43-9006, it is the first oral multikinase inhibitor designed to target both tumor cell signaling and angiogenesis. Sorafenib was subsequently approved for the treatment of liver cancer in 2007 and thyroid cancer in 2013. Sorafenib is an oral multi-kinase inhibitor used as targeted therapy for advanced cancers such as hepatocellular carcinoma (liver cancer), renal cell carcinoma (kidney cancer), and differentiated thyroid cancer. It works by blocking multiple kinases involved in cancer cell proliferation and the formation of new blood vessels (angiogenesis), thereby inhibiting tumor growth and potentially killing cancer cells. Sorafenib is typically taken as a tablet twice daily, either on an empty stomach or with a low-fat meal.
BRAND NAMES
The most well-known brand name for the cancer drug sorafenib is Nexavar.
Other brand names for sorafenib include:
Sorafenat
Soranib
Sorabuzz
Cadsonib
Sorepto
Soratib
MECHANISM OF ACTION
Sorafenib exerts its effects through a dual mechanism of action by inhibiting both tumor cell proliferation and tumor angiogenesis. It blocks the RAF/MEK/ERK signaling pathway within cancer cells, halting their division and growth, while also inhibiting VEGFR and PDGFR pathways, which are essential for the formation of new blood vessels that supply tumors. By targeting these multiple kinases, sorafenib effectively suppresses tumor growth and promotes cancer cell death.
PHARMACOKINETICS
Absorption
Sorafenib’s oral absorption is limited due to its low water solubility, placing it in Class II of the biopharmaceutical classification system. After administration, it is absorbed through the gastrointestinal tract, with peak plasma concentrations usually reached within 1 to 12 hours.
Distribution
For an average 80 kg patient, the approximate volume of distribution for sorafenib is 213 liters, with a reported range of 50 to 1,000 liters.
Metabolism
Sorafenib is primarily metabolized in the liver via two main pathways: oxidative metabolism by the enzyme CYP3A4 and glucuronidation by UGT1A9. This metabolism produces several metabolites, and the majority of the drug is eliminated through biliary excretion into the feces, with a smaller portion excreted in the urine.
Excretion
Sorafenib is primarily excreted in the feces, with about 77% of the dose eliminated this way, mostly as unchanged drug. Approximately 19% is excreted in the urine, mainly in the form of glucuronidated metabolites. Before excretion, sorafenib undergoes extensive metabolism in the liver.
PHARMACODYNAMICS
Sorafenib is an oral multikinase inhibitor with dual pharmacodynamic effects: it blocks the proliferation of tumor cells and inhibits the formation of new blood vessels (angiogenesis) that feed the tumor. Its anti-cancer activity results from targeting a wide range of serine/threonine and receptor tyrosine kinases crucial for multiple signaling pathways.
ADMINISTRATION
Sorafenib is administered orally in the form of tablets. The typical dose for adults is 400 mg taken twice daily (total 800 mg per day), with or without a low-fat meal to improve tolerability. It’s important to swallow the tablets whole with water and not to crush or chew them. The dosing schedule may be adjusted based on individual patient response, tolerance, and the presence of side effects. Regular monitoring by a healthcare provider is essential to manage any adverse effects and to assess treatment effectiveness.
DOSAGE AND STRENGTH
Sorafenib is typically prescribed at a dose of 400 mg taken orally twice daily (total daily dose of 800 mg). It is available in tablet form, commonly in strengths of 200 mg. Patients usually take two 200 mg tablets per dose, with or without a low-fat meal. Dosage adjustments may be necessary based on tolerance, side effects, or specific patient conditions as determined by the healthcare provider.
FOOD INTERACTIONS
Sorafenib’s absorption can be affected by food. Taking sorafenib with a high-fat meal may reduce its bioavailability, so it is generally recommended to take the medication either on an empty stomach or with a low-fat meal to ensure consistent absorption. Patients should follow their healthcare provider’s instructions regarding food intake to optimize the drug’s effectiveness.
DRUG INTERACTIONS
Sorafenib interacts with several drugs, including CYP3A4 inhibitors and inducers that can increase or decrease its levels, affecting effectiveness and toxicity. It may also increase the risk of heart rhythm problems when combined with QT-prolonging drugs and can raise bleeding risk when taken with anticoagulants. Close monitoring and careful management of all medications are important to avoid adverse interactions.
CONTRAINDICATIONS
Sorafenib is contraindicated in patients with severe hypersensitivity to the drug or any of its components and is not recommended to be used alongside certain other cancer therapies. Caution or avoidance is advised in individuals with specific cardiovascular conditions, severe liver impairment, and certain types of lung cancer due to potential safety risks.
SIDE EFFECTS
Hand-foot skin reaction (HFSR).
Diarrhea.
Fatigue and weakness.
Rash.
High blood pressure (hypertension).
Weight and appetite changes.
Hair loss or thinning (alopecia).
Bleeding.
Heart problems.
Heart rhythm changes.
Liver damage.
Gastrointestinal perforation.
Wound healing issues.
Hypothyroidism.
OVERDOSE
Severe diarrhea.
High blood pressure (hypertension).
Extreme fatigue or weakness.
Nausea and vomiting.
Severe skin reactions.
Loss of appetite and weight loss.
Abdominal pain.
Dizziness or headache.
Cardiac arrhythmias or palpitations.
Bleeding or bruising.
Liver dysfunction.
TOXICITY
Sorafenib toxicity commonly presents with gastrointestinal issues such as diarrhea and hand-foot skin reaction (HFSR), along with hypertension and fatigue. Less frequently, serious toxicities like liver injury and cardiac complications may occur. Management typically involves dose adjustments, proactive measures such as using skin creams and anti-diarrheal medications, and regular medical monitoring to detect and address side effects promptly.