Sevoflurane was first patented in 1972 by Ross Terrell and Richard Wallen. Its clinical use began in Japan in 1990 through Maruishi Pharmaceuticals. The drug received FDA approval in 1996 and was subsequently marketed worldwide by Abbott Laboratories under the trade names Ultane® and Sevorane®, with generic formulations becoming available around 2006. Sevoflurane is a widely used inhaled anesthetic for general anesthesia, appreciated for its rapid onset, smooth induction, and quick recovery profile. Administered via a specialized vaporizer, it is particularly advantageous in pediatric and outpatient settings due to its excellent tolerability and minimal airway irritation compared with older anesthetic agents. Its primary applications include the induction and maintenance of general anesthesia during surgical and procedural interventions.
BRAND NAMES
Ultane.
Sevorane.
Sojourn.
Sevura.
Sevitrue.
MECHANISM OF ACTION
The exact mechanism of action of sevoflurane is not completely understood, but it is thought to produce general anesthesia by interacting with multiple receptor systems in the central nervous system. It enhances inhibitory neurotransmission through its actions on GABA and glycine receptors, while suppressing excitatory neurotransmission by modulating nicotinic acetylcholine, serotonin, and glutamate receptors. Additionally, sevoflurane influences voltage gated and two-pore potassium channels, which further contribute to its anesthetic properties.
PHARMACOKINETICS
Absorption
Sevoflurane is rapidly absorbed through the lungs into the bloodstream because of its low blood solubility (blood/gas partition coefficient of approximately 0.69), enabling faster induction and recovery from anesthesia compared with older inhalational agents. The rate of absorption depends on several factors, including the inspired concentration, partition coefficients, minute ventilation, and pulmonary blood flow.
Distribution
Sevoflurane has a volume of distribution of approximately 53 liters; however, its rapid uptake and elimination are more clinically relevant characteristics. These properties are largely determined by its low blood/gas partition coefficient (about 0.63–0.69), which facilitates swift induction and recovery during anesthesia.
Metabolism
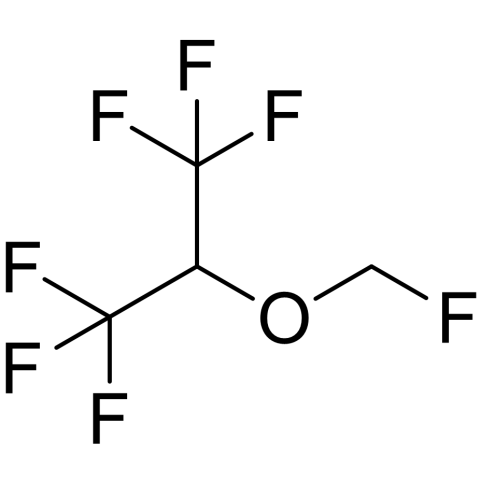
Sevoflurane is metabolized in the liver by the enzyme cytochrome P450 2E1, with about 2% to 5% of the administered dose broken down into inorganic fluoride and hexafluoroisopropanol (HFIP). HFIP is rapidly conjugated with glucuronic acid and excreted in the urine, while inorganic fluoride is also eliminated via urine or may be taken up by bone. The majority of sevoflurane is eliminated unchanged through the lungs, which serves as its primary route of elimination.
Elimination
Sevoflurane excretion primarily occurs through the lungs, where the majority of the anesthetic is eliminated unchanged by exhalation. A small portion (about 2% to 5%) is metabolized in the liver to inorganic fluoride and hexafluoroisopropanol (HFIP).
PHARMACODYNAMICS
Sevoflurane’s pharmacodynamics involve dose-dependent depression of the central nervous system, cardiovascular system, and respiratory system by enhancing inhibitory neurotransmission and inhibiting excitatory neurotransmission. Its low blood solubility contributes to rapid induction and emergence from anesthesia. Additionally, its minimal airway irritant properties make it well-suited for mask induction, particularly in pediatric patients. Factors such as age significantly influence its effects, with older patients requiring a lower minimum alveolar concentration to achieve anesthesia.
DOSAGE AND ADMINISTRATION
Sevoflurane is administered as an inhaled anesthetic through a specialized vaporizer, typically delivered via face mask, endotracheal tube, or laryngeal mask airway during general anesthesia. For induction, sevoflurane is usually started at an inspired concentration of 2% to 8%, with pediatric patients often benefiting from its low airway irritation during mask induction. In adults, induction concentrations generally range from 3% to 8%. Maintenance doses typically range from 1% to 3%, adjusted based on the patient’s age, procedure, and anesthetic depth required. The minimum alveolar concentration of sevoflurane varies with age, decreasing in elderly patients, and dosage adjustments may be necessary for those with cardiovascular or respiratory compromise. Sevoflurane is often used in combination with other anesthetics and analgesics as part of balanced anesthesia. Continuous monitoring of vital signs, oxygen saturation, end-tidal CO₂, and anesthesia depth is essential to ensure safety and effectiveness during administration.
FOOD INTERACTIONS
There are no known direct food interactions with sevoflurane; however, patients undergoing general anesthesia with sevoflurane must strictly follow preoperative fasting guidelines to reduce the risk of serious complications during surgery. The primary precaution regarding interactions is that alcohol consumption should be avoided, as it may affect anesthesia safety and effectiveness.
DRUG INTERACTIONS
Sevoflurane can interact with several drugs, including CYP450 inhibitors like cimetidine that may increase its effects, and CNS depressants such as opioids or benzodiazepines, which can enhance sedation and respiratory depression. It also potentiates neuromuscular blockers, leading to prolonged muscle relaxation. Although less common, caution is needed with drugs that sensitize the heart to catecholamines due to potential arrhythmias. Alcohol should be avoided as it may increase CNS depression and affect anesthesia safety. Careful monitoring is important when sevoflurane is used alongside other medications.
CONTRAINDICATIONS
Sevoflurane is contraindicated in patients with known or suspected sensitivity to sevoflurane or other halogenated anesthetics. It is also contraindicated in individuals susceptible to malignant hyperthermia, as well as those with certain liver or heart conditions.
SIDE EFFECTS
Common side effects:
Nausea and vomiting.
Agitation, confusion, or delirium.
Dizziness, lightheadedness, or drowsiness.
Changes in blood pressure.
Changes in heart rate (can be fast or slow).
Headache.
Cough.
Fever or chills.
Low body temperature.
Serious side effects:
Malignant hyperthermia.
Allergic reaction.
Breathing problems.
Cardiovascular issues.
Liver problems.
Seizures .
Kidney problems.
OVERDOSE
Respiratory depression: Slow, shallow, or labored breathing, or complete cessation of breathing (apnea).
Cardiovascular collapse: This can involve a significant drop in blood pressure (hypotension), a slow heart rate (bradycardia), or cardiac arrest.
Central nervous system depression: Confusion, agitation, seizures, and loss of consciousness.
Other symptoms: Nausea, vomiting, and a potential risk for kidney or liver injury.
TOXICITY
Sevoflurane toxicity may cause hepatotoxicity, nephrotoxicity, and neurotoxicity. Potential adverse effects include renal injury, respiratory depression, QT prolongation, and malignant hyperthermia. In pediatric patients, there is particular concern about neurotoxicity, as well as a risk of severe bradycardia and cardiac arrest in those with Down syndrome. The risk of renal toxicity is linked to the formation of compound A during anesthesia, especially under low fresh gas flow conditions, which the FDA advises against for certain procedures to minimize this risk.