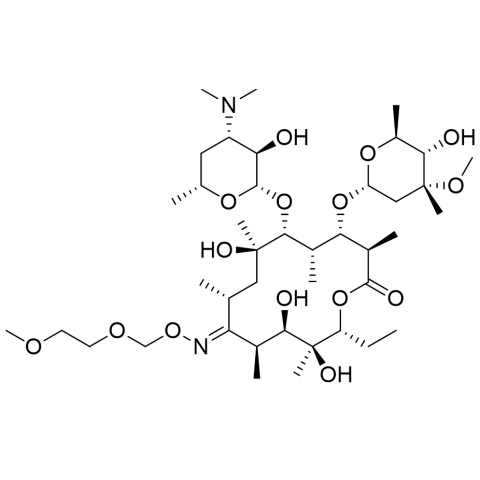
Roxithromycin is a semi-synthetic macrolide antibiotic derived from erythromycin, developed in the 1980s by the German pharmaceutical company Hoechst Uclaf. Its development started in 1980, and it was approved for medical use in 1987, with a patent granted in the same year. Designed to improve on erythromycin, roxithromycin has enhanced stability and a broader spectrum of activity against various bacterial infections, including respiratory tract infections, skin infections, and urinary tract infections. It is widely marketed under different brand names in several countries, though it is not approved for use in the United States. Roxithromycin works by inhibiting bacterial protein synthesis, making it effective against both Gram-positive and some Gram-negative bacteria, and it is generally well tolerated with a lower incidence of gastrointestinal side effects compared to erythromycin.
BRAND NAMES
Roxithromycin is marketed under several brand names worldwide. The most commonly known brand is Rulid, which is available in tablet form. Other brands include Roxit, Roximycin, Rulide, and Roxim. Brand names may vary by country and formulation. These brands make it easier for patients and prescribers to identify the medication.
MECHANISM OF ACTION
Roxithromycin works by binding to the 50S ribosomal subunit of susceptible bacteria. This inhibits protein synthesis, preventing bacterial growth and replication. It acts primarily as a bacteriostatic agent, although high concentrations may be bactericidal. Its mechanism targets Gram-positive bacteria and some Gram-negative strains. This dual activity makes it effective in respiratory, skin, and soft tissue infections.
PHARMACOKINETICS:
Absorption
Roxithromycin is rapidly absorbed after oral administration. Peak plasma concentrations occur within 1–2 hours. Taking it with food can enhance absorption slightly. Its bioavailability is high, allowing effective systemic concentrations. The absorption rate supports once- or twice-daily dosing.
Distribution
The drug distributes widely into body tissues, including lungs, tonsils, and sinuses. Low plasma protein binding allows greater free drug availability. Tissue concentrations often exceed plasma levels, enhancing efficacy. Roxithromycin crosses the placenta but minimally enters cerebrospinal fluid. Distribution is consistent in most adult populations.
Metabolism
Roxithromycin undergoes partial metabolism in the liver through demethylation and oxidation. Minor metabolites have little antibacterial activity. Metabolism is not heavily dependent on CYP450 enzymes, reducing drug interactions. Liver function can influence the rate of metabolism. The drug maintains effective plasma levels for once- or twice-daily dosing.
Excretion
Roxithromycin is primarily excreted in bile and feces, with minimal renal excretion. The half-life supports convenient dosing schedules. Clearance may be slower in patients with hepatic impairment. Less than 10% of the drug is excreted unchanged in urine. This excretion profile minimizes accumulation in patients with normal liver function.
PHARMACODYNAMICS
Roxithromycin exerts bacteriostatic effects by inhibiting bacterial protein synthesis. Its activity is concentration-dependent and time-dependent, requiring consistent dosing. Effective against Gram-positive bacteria and selected Gram-negative species. It reduces bacterial load and indirectly decreases inflammation. Its clinical use focuses on respiratory, skin, and soft tissue infections.
ADMINISTRATION
Roxithromycin is administered orally, either as tablets or suspension. It can be taken with or without food for convenience. The standard dosing frequency is once or twice daily depending on infection severity. Patients are advised to complete the full course to prevent resistance. Adjustments may be necessary in hepatic impairment.
DOSAGE AND STRENGTH
Typical adult doses range from 150–300 mg twice daily depending on the infection. Pediatric dosing is weight-based, usually 5–8 mg/kg/day. Tablets are available in 150 mg and 300 mg strengths. Oral suspension is commonly 50 mg/5 mL. Treatment duration generally ranges from 7–10 days, depending on the infection type.
DRUG INTERACTIONS
Roxithromycin may interact with warfarin, theophylline, and cyclosporine. Caution is advised with other CYP3A4-metabolized drugs. Co-administration with other macrolides may increase the risk of side effects. Monitoring is recommended for drugs that prolong QT interval. Always check for interactions before starting therapy.
FOOD INTERACTIONS
Food slightly enhances absorption but is not critical for effectiveness. Fatty meals may delay peak plasma concentrations. No strict dietary restrictions are necessary. Alcohol does not significantly affect pharmacokinetics. Hydration can reduce gastrointestinal discomfort during therapy.
CONTRAINDICATIONS
Roxithromycin is contraindicated in patients with hypersensitivity to macrolides or erythromycin. Patients with a history of cholestatic jaundice from macrolides should avoid it. Severe hepatic impairment warrants caution or dose adjustment. Pre-existing QT prolongation is a concern. Avoid use in patients with known allergy to any formulation of Roxithromycin.
SIDE EFFECTS
Nausea, vomiting, and diarrhea
Abdominal cramps and discomfort
Headache or dizziness
Skin rash or allergic reactions
Rare liver enzyme elevation or jaundice
OVER DOSE
Excessive ingestion may lead to gastrointestinal symptoms like nausea, vomiting, and diarrhea. Severe cases can cause bradycardia or hypotension. Supportive treatment is recommended. Liver and kidney function should be monitored. No specific antidote exists; management is symptomatic.
TOXICITY
Roxithromycin toxicity is usually dose-dependent and reversible. High doses may cause hepatotoxicity or liver enzyme elevation. Prolonged QT interval may occur in predisposed individuals. Allergic reactions are rare but possible. Proper dosing and monitoring minimize serious adverse events.