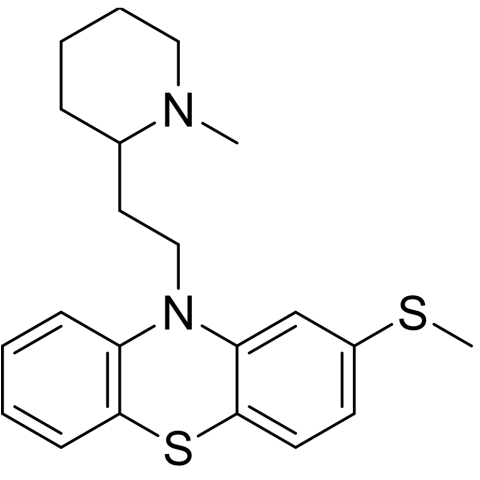
Thioridazine is a first-generation (typical) antipsychotic that was once widely used to treat schizophrenia but is now prescribed less often due to significant side effects, particularly its dose-dependent risk of QTc interval prolongation and sudden cardiac death. It works by targeting dopamine receptors to control psychotic symptoms, but its use is now mostly limited to patients who do not respond to or cannot tolerate other antipsychotic medications. Its prescription is further limited by genetic variations in the CYP2D6 enzyme, which can lead to elevated drug levels and heightened cardiac risks. Thioridazine is available in tablet form and has also been explored as a potential treatment for drug-resistant tuberculosis due to its antimicrobial properties.
BRAND NAMES:
Thioridazine, marketed under brand names such as Mellaril or Melleril, is a typical antipsychotic from the phenothiazine class. It was once commonly prescribed for managing schizophrenia and other psychotic disorders.
MECHANISM OF ACTION:
Thioridazine works by blocking postsynaptic D1 and D2 dopamine receptors in the mesolimbic pathway of the brain. It also inhibits alpha-adrenergic activity, reduces the secretion of hormones from the hypothalamus and pituitary gland, and is thought to suppress the reticular activating system. As a result, it influences functions such as basal metabolic rate, body temperature regulation, alertness, blood vessel tone, and the vomiting reflex.
PHARMACOKINETICS
Absorption:
Thioridazine is efficiently absorbed after oral intake. Being lipophilic, it disperses widely throughout body tissues. Like other drugs in the phenothiazine class, it undergoes extensive hepatic metabolism, resulting in the formation of numerous metabolites.
Distribution:
The drug and its active metabolites particularly mesoridazine are extensively distributed across the body, including the central nervous system, as they can cross the blood-brain barrier. Although thioridazine tends to have lower plasma concentrations compared to its metabolites, it accumulates in the brain at much higher levels.
Metabolism:
Thioridazine is extensively metabolized in the liver, with its main pathway involving oxidation by the cytochrome P450 (CYP450) enzyme system, particularly CYP2D6. This process produces several metabolites, some of which are pharmacologically active and more potent than the parent drug.
Excretion:
Thioridazine is extensively metabolized by the liver, primarily by the cytochrome P450 2D6 (CYP2D6) enzyme, before its metabolites are excreted mainly through the feces. Renal excretion plays a significantly smaller role in its elimination.
PHARMACODYNAMICS
Thioridazine is a first-generation antipsychotic and phenothiazine derivative with a complex mechanism of action involving multiple neurotransmitter systems in the central nervous system. Its activity is primarily based on blocking postsynaptic receptors, but it also causes a range of side effects due to its interactions with other receptors.
ADMINISTRATION
Thioridazine is administered orally in tablet form, with the dosage tailored to the individual patient based on their condition and response to treatment. It is usually given in divided doses throughout the day and can be taken with or without food. Due to its potential for serious cardiac side effects, such as QTc prolongation, its use is limited to patients who have not responded to other antipsychotics. Close medical supervision and regular monitoring are essential during treatment.
DOSAGE AND STRENGTH
Thioridazine is available in oral tablet form with strengths typically including 10 mg, 25 mg, 50 mg, 100 mg, and 200 mg. The dosage is individualized based on the patient's condition, age, and response to therapy. For adults with schizophrenia or psychotic disorders, initial doses usually range from 50 mg to 100 mg three times daily, with gradual adjustments as needed.
DRUG INTERACTIONS
Medications that inhibit CYP450 2D6 should be used with caution when prescribing thioridazine. Medications that may affect thioridazine levels include but are not limited to fluoxetine, paroxetine, duloxetine, fluvoxamine, propranolol, citalopram, and pindolol.
FOOD INTERACTIONS
Thioridazine has significant food interactions, requiring that you avoid alcohol because it can increase central nervous system depression and side effects like dizziness and falls. Caffeine intake should be limited, as it may raise blood pressure and affect the way the medication is metabolized in the body. Although not a food, patients should be cautious with vitamin A supplements, as thioridazine may elevate vitamin A levels, leading to potential toxicity.
CONTRAINDICATIONS
patients with long QT syndrome, QT intervals prolonged to more than 450, or taking concomitant medications known to prolong the QT interval should avoid thioridazine. Additionally, individuals with a history of heart arrhythmias or heart conditions related to low or high blood pressure should refrain from using this medication.
SIDE EFFECTS
drowsiness
blurred vision
dry mouth
nausea
vomiting
diarrhea
constipation
changes in appetite
weight gain
stuffed nose
pale skin
darkening of the skin or eyes
Swelling may occur in the arms, hands, feet, ankles, or lower legs.
blank facial expression
shuffling walk
Abnormal, slowed, or involuntary movements in any part of the body.
restlessness
SERIOUS SIDE EFFECTS:
fever
muscle stiffness
confusion
sweating
neck cramps
tightness in the throat
difficulty breathing or swallowing
tongue that sticks out of the mouth
fine, worm-like tongue movements
uncontrollable, rhythmic face, mouth, or jaw movements
vision loss, especially at night
seeing everything with a brown tint
yellowing of the skin and eyes
rash
OVER DOSE
Severe drowsiness or coma
Confusion or agitation
Seizures
Respiratory depression
Irregular heartbeat or arrhythmias, especially QTc prolongation and torsades de pointes
Hypotension (low blood pressure)
Dry mouth, difficulty urinating, blurred vision, and constipation.
TOXICITY
Thioridazine toxicity primarily manifests as severe, vision-threatening pigmentary retinopathy, with symptoms including blurred vision, night blindness (nyctalopia), and dyschromatopsia (altered colour vision). Toxicity risk increases with higher daily doses, particularly above 800 mg/day, and can develop within weeks of starting therapy.